Diuretic and Anti-Inflammatory Pill vs. Pelvic Therapy for Chronic Prostatitis
Chronic prostatitis, often termed chronic pelvic pain syndrome (CP/CPPS), affects millions of men with persistent pelvic pain, urinary difficulties, and emotional distress. For chronic sufferers, finding effective, long-term relief is a priority. Two distinct approaches—the Diuretic and Anti-Inflammatory Pill, a traditional Chinese medicine (TCM) formula, and Pelvic Floor Physical Therapy, a musculoskeletal-focused treatment—offer promising options. This article compares their mechanisms, benefits, and limitations to help chronic prostatitis patients choose the best path for relief.
Understanding Chronic Prostatitis
Chronic prostatitis (CP/CPPS) is defined by pelvic pain lasting at least three months, often accompanied by urinary symptoms like urgency, frequency, or discomfort, and sometimes sexual dysfunction. It affects 10-15% of men, significantly impacting quality of life [1]. Causes are complex, including inflammation, pelvic floor muscle dysfunction, nerve irritation, or stress, making treatment challenging. Antibiotics are ineffective for non-bacterial cases, which comprise 90-95% of CP/CPPS, and drugs like alpha-blockers often provide only temporary relief. This complexity drives interest in alternative treatments like the Diuretic and Anti-Inflammatory Pill and pelvic floor therapy.
Overview of Treatment Options
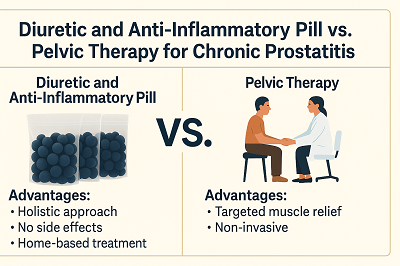
Diuretic and Anti-Inflammatory Pill is a TCM formula with over 50 herbs, designed to address inflammation, blood stasis, pain, and urinary issues holistically. It’s taken at home, offering convenience for chronic management. In contrast, Pelvic Floor Physical Therapy involves targeted exercises, biofeedback, and manual techniques to relieve pelvic muscle tension, typically administered by a specialized therapist. Both approaches target chronic prostatitis but differ in scope and delivery, making a comparison essential for informed decision-making.
How Diuretic and Anti-Inflammatory Pill Works
The Diuretic and Anti-Inflammatory Pill takes a multi-targeted approach to chronic prostatitis:
Anti-Inflammatory: Herbs like Safflower and Angelica Sinensis reduce inflammation in the prostate and pelvic tissues, a key CP/CPPS driver.
Blood Circulation: Peach Kernel and Radix Paeoniae Rubra enhance blood flow, preventing stasis and aiding tissue repair.
Pain Relief: Houttuynia Cordata and Corydalis Yanhusuo relax pelvic muscles and ease neuropathic pain, addressing discomfort in the pelvis or perineum.
Urinary Function: Plantain Seed and Talcum act as diuretics, clearing urinary tract irritation to improve flow and reduce urgency.
How Pelvic Floor Physical Therapy Works
Pelvic Floor Physical Therapy focuses on musculoskeletal issues common in CP/CPPS, particularly pelvic floor muscle hypertonicity [2]. Its mechanisms include:
Muscle Relaxation: Exercises like Kegels or stretching reduce pelvic floor muscle tension, alleviating pain and improving function [3].
Biofeedback: Tools help patients control pelvic muscles, enhancing coordination and reducing spasms.
Circulatory Benefits: Therapy improves pelvic blood flow, indirectly supporting symptom relief.
Therapy requires weekly or bi-weekly sessions with a trained therapist, plus home exercises. Studies show significant symptom improvement in some CP/CPPS patients, particularly those with pelvic floor spasms, with a 50% response rate in comprehensive programs [4]. However, its focus on muscles limits its impact on inflammation or urinary symptoms.
Comparing Advantages and Limitations
Diuretic and Anti-Inflammatory Pill
Advantages:
Multi-Targeted: Addresses inflammation, pain, and urinary issues holistically, ideal for CP/CPPS's complexity.
No Side Effects: Unlike antibiotics, it is gentle, supporting long-term use for chronic patients.
Convenience: Home-based treatment eliminates the need for frequent appointments.
Broad Applicability: May benefit related conditions like epididymitis or urinary tract issues.
Limitations:
Gradual Results: Typically takes 1–3 months to achieve full effect, as the treatment works steadily to eliminate inflammation at its root—requiring some patience but offering more lasting relief.
Pelvic Floor Physical Therapy
Advantages:
Targeted Muscle Relief: Effective for pelvic floor dysfunction, a key CP/CPPS factor, with evidence of pain reduction [3].
Non-Invasive: No medications or side effects, appealing for chronic management.
Research-Backed: Studies confirm efficacy for muscle-related symptoms [4].
Limitations:
Limited Scope: Primarily addresses muscle tension, not inflammation or urinary issues [2].
Time and Cost: Requires ongoing professional sessions, less convenient for chronic patients.
Variable Outcomes: Success depends on therapist expertise and patient compliance [4].
Why Diuretic and Anti-Inflammatory Pill Suits Chronic Patients
For chronic prostatitis sufferers, the Diuretic and Anti-Inflammatory Pill offers distinct advantages. Its holistic approach tackles multiple CP/CPPS aspects—inflammation, pain, and urinary dysfunction—making it ideal for complex, long-term cases. Unlike pelvic floor therapy, which requires regular therapist visits, the pill's home-based administration fits busy lifestyles, a critical factor for chronic patients. Its lack of side effects supports extended use, avoiding issues like antibiotic resistance [1]. Additionally, it can complement lifestyle changes or even physical therapy for enhanced results, offering flexibility.
Practical Considerations for Chronic Prostatitis Patients
When choosing between these treatments, consider:
Symptom Profile: Opt for the Diuretic and Anti-Inflammatory Pill if inflammation or urinary issues predominate; choose pelvic floor therapy for muscle-related pain.
Lifestyle: Home-based pill suits those with limited time; therapy requires session commitments.
Professional Guidance: Consult a TCM practitioner for the pill or a physical therapist for therapy.
Lifestyle Support:
Diet: Avoid caffeine and spicy foods; include anti-inflammatory foods like berries.
Exercise: Gentle yoga or stretching complements both treatments.
Stress Management: Mindfulness reduces symptom triggers.
Conclusion
The Diuretic and Anti-Inflammatory Pill and Pelvic Floor Physical Therapy offer valuable approaches to chronic prostatitis, but their strengths differ. The pill's holistic, home-based treatment excels for chronic patients needing comprehensive relief from inflammation, pain, and urinary issues. Pelvic floor therapy shines for muscle-related symptoms but is less versatile and more time-intensive.
Chronic sufferers may find the Diuretic and Anti-Inflammatory Pill's convenience and multi-targeted effects ideal, potentially combined with lifestyle changes or therapy for optimal results. Consult a TCM practitioner to explore this herbal remedy and take control of your chronic prostatitis.
References
[1] National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2023). Prostatitis: Inflammation of the Prostate. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostatitis-inflammation-prostate
[2] Yani, M. S., Eckel, S. P., Kirages, D. J., Rodriguez, L. V., Corcos, D. M., & Kutch, J. J. (2022). Impaired ability to relax pelvic floor muscles in men with chronic prostatitis/chronic pelvic pain syndrome. Physical Therapy, 102(7), pzac053. https://doi.org/10.1093/ptj/pzac053
[3] Van Alstyne, L. S., Harrington, K. L., & Haskvitz, E. M. (2010). Physical therapist management of chronic prostatitis/chronic pelvic pain syndrome. Physical Therapy, 90(12), 1795–1806. https://pubmed.ncbi.nlm.nih.gov/20864601/
[4] Masterson, T. A., Patel, P., Woolford, J., Cohn, J. A., & Gonzalez, C. M. (2017). Comprehensive pelvic floor physical therapy program for men with idiopathic chronic pelvic pain syndrome: A prospective study. Translational Andrology and Urology, 6(5), 910–915. https://doi.org/10.21037/tau.2017.08.17



