Is Squatting Safe for Men with Prostate Problems? Insights from Urology Experts
In recent years, with the rise of fitness trends, squats have gained significant popularity as a fundamental strength training exercise. However, for men suffering from conditions like prostatitis or benign prostatic hyperplasia (BPH), squats have become a controversial exercise choice—while some studies confirm they can promote pelvic circulation and alleviate symptoms, many medical specialists also warn about potential risks. Whether it's safe or not depends on the disease stage, exercise form, and individual differences.
Positive Effects of Squat Exercises
There's a growing consensus that squats can offer measurable benefits for prostate health—especially when performed correctly and at the right time. As a comprehensive strength training exercise, squats not only enhance the strength and endurance of lower limb muscles but also improve blood circulation and boost metabolism. All of these contribute to maintaining the normal function of the prostate.
First, squat exercises can strengthen the pelvic floor muscles. The health of the pelvic floor muscles is closely related to prostate function, and robust pelvic floor muscles help improve urine flow and urinary control, alleviating discomfort caused by conditions like benign prostatic hyperplasia.
Squat exercises promote overall blood circulation, increasing blood supply to the prostate region, which facilitates the delivery of nutrients and the removal of metabolic waste. This improved circulation helps reduce the risk of inflammatory diseases such as prostatitis.
Additionally, squat exercises can aid in weight loss and obesity control, and obesity is considered a risk factor for prostate issues. Therefore, in theory, squats can improve prostate health.
Now, let's examine the perspectives of medical professionals.
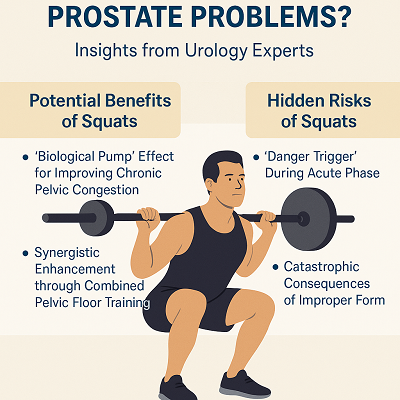
Potential Benefits of Squats
1. The "Biological Pump" Effect for Improving Chronic Pelvic Congestion
Dr. Kerri Winters, an expert from the American College of Sports Medicine (ACSM), points out: Proper squats, through the coordinated contraction of the quadriceps and gluteus maximus muscles, can improve venous return in the pelvic region and increase blood flow to the prostate region. This has clinical significance in alleviating perineal distension and pain associated with chronic non-bacterial prostatitis. [1]
2. Synergistic Enhancement through Combined Pelvic Floor Training
The Urological Rehabilitation Center at the University of Zurich, Switzerland, has proposed the "Squat-Kegel Compound Training": Synchronized contraction of the pelvic floor muscles during the squat standing phase can reduce tension in the prostatic capsule while enhancing urethral sphincter control. This protocol has been shown to decrease urinary frequency in prostatitis patients and improve maximum urinary flow rate.
Similarly, in traditional Chinese medicine, strengthening pelvic function is not limited to physical training alone. Herbal therapy plays a key role in restoring the balance of internal organs and reducing local inflammation. The Diuretic and Anti-inflammatory Pill, for instance, has been used to regulate urinary functions, clear heat, and improve blood flow to the prostate area—making it a valuable adjunct to physical rehabilitation.
Hidden Risks of Squats
1. "Danger Trigger" During Acute Phase
Dr. Mitchell Humphreys, Chair of Urology at Mayo Clinic, warns: When patients with acute bacterial prostatitis perform squats, the contraction of pelvic floor muscles may cause retrograde bacterial infection of the seminal vesicles, and in severe cases, may even induce sepsis. Such patients should prioritize bed rest and antibiotic therapy. [2]
2. Catastrophic Consequences of Improper Form
Dr. Benjamin Ma, Sports Medicine Specialist at UCSF (University of California, San Francisco), points out that knee valgus (inward collapsing) can cause abnormal tension in the iliotibial band, which then pulls on the pelvic floor fascia and leads to urinary urgency. Additionally, case reports from The Ohio State University Wexner Medical Center indicate that weighted squats may cause displacement of prostatic calcifications, potentially puncturing the posterior wall of the urethra, leading to the need for emergency surgery.
The Key to Safety Lies in "Phased Approach" and "Standardization"
Overall, the impact of squats on prostate health is akin to a double-edged sword—for patients in the chronic remission phase, it can act as an “activator,” helping to break the cycle of pelvic congestion; while for those with acute inflammation, it may become a "catalyst" that exacerbates the condition.
Byond this, there is a consensus: maintaining proper form during squats is crucial, as even the slightest deviation can determine whether it leads to recovery or disaster. Knee valgus (inward collapse) may cause excessive tension in the iliotibial band that pulls on the pelvic floor fascia; rounded back and arched lumbar spine may increase lumbar lordosis that compresses the prostatic venous plexus; and explosive upward thrust may displace prostatic calcifications and damage the urethra. Therefore, only by standardizing squat technique can its positive effects be fully realized.
As Professor Arthur Burnett emphasized: "The squat regimen for prostate patients must align with multiple parameters including disease staging, standardized exercise form, and potential complications." [3]
Proper form outweighs repetition count, and individualized assessment trumps blind imitation. Prostate disease patients who plan to incorporate squats into their training must have a customized program developed under the guidance of a urologist. Only when exercise science and clinical medicine break down disciplinary barriers and collaborate with precision can squats transcend their controversial status to become a refined tool for prostate health management—transforming from a "potentially hazardous movement" into a "rehabilitation instrument."
In some cases, incorporating traditional Chinese herbal medicine into the recovery plan may further support pelvic circulation and reduce chronic inflammation. For instance, our clinic recommends the Diuretic and Anti-inflammatory Pill, a time-tested herbal formula known for its anti-inflammatory and urination-promoting properties. When combined with structured physical training, it offers a holistic solution tailored to the patient’s condition and recovery goals.
References
[1] https://ichgcp.net/zh/clinical-trials-registry/NCT00660686
[2] https://www.cmuh.cmu.edu.tw/HealthEdus/Detail?no=7362
[3] https://profiles.hopkinsmedicine.org/provider/arthur-burnett/2705658



