How Caffeine Triggers Prostatitis Flare-ups and How to Cope
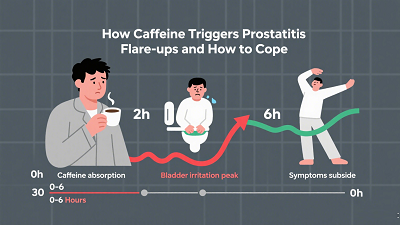
If you live with prostatitis—especially the chronic form marked by pelvic pain and urinary symptoms—you may have noticed a pattern: a strong coffee or two, and your symptoms ramp up. Many men report that caffeine worsens frequency, urgency, burning with urination, or pelvic discomfort. But why does this happen, and what’s the smartest way to cope without feeling like you have to give up everything you enjoy? This guide explains the mechanisms that may link caffeine to prostatitis flare-ups, what the research does (and doesn’t) say, and practical strategies that genuinely help.
Prostatitis in One Minute: What You’re Managing
Prostatitis is a broad term:
Acute or chronic bacterial prostatitis: driven by infection and typically treated with antibiotics.
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS): the most common form, involving pelvic pain and urinary symptoms for 3 months or longer without a clear infection.
Flares in CP/CPPS can be triggered by multiple factors—stress, constipation, vigorous exercise, sexual activity changes, and yes, beverages and foods that irritate the bladder. That’s where caffeine often comes in.
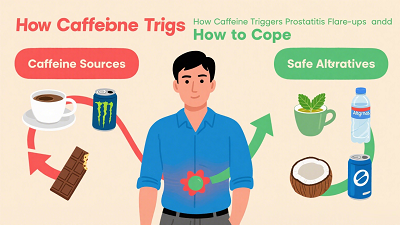
How Caffeine Can Trigger Prostatitis Flare-ups
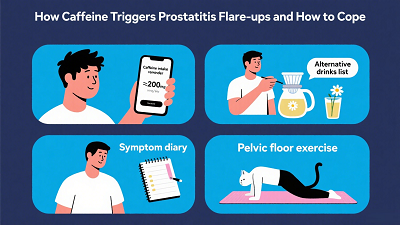
Caffeine doesn’t cause prostatitis on its own, but it can aggravate the urinary and pelvic symptoms that define a flare. Several plausible mechanisms help explain why:
Bladder and urethral irritation: Caffeinated drinks can make you feel the need to urinate more often and more urgently. When your bladder is more active and your urethra feels irritated, the prostate and the pelvic floor can become reactive, heightening pain and burning sensations.
Mild diuretic effect: For some people—especially those not used to caffeine—caffeine can increase urine production. More trips to the bathroom can lead to more urethral and pelvic floor irritation during a flare.
Increased sympathetic tone: Caffeine blocks adenosine receptors, which can raise alertness and sympathetic (“fight-or-flight”) activity. In susceptible individuals, this may tighten the pelvic floor and the bladder neck, worsening a sense of fullness, urgency, or incomplete emptying.
Sleep and pain sensitivity: Late-day caffeine can disrupt sleep. Poor sleep amplifies pain sensitivity and stress, both known flare triggers in CP/CPPS.
Individual thresholds: People vary widely in how they metabolize caffeine. One person may tolerate two espressos; another flares after a single cup of tea. Tracking your personal threshold is key.
What the Research Says—and What It Doesn’t
Direct, high-quality research tying caffeine to prostatitis flare-ups is limited. However, there is relevant research linking higher caffeine intake with urinary symptoms in a related prostate condition. A cross-sectional study using U.S. NHANES data found that men with higher caffeine intake had higher odds of benign prostatic hyperplasia (BPH), even after adjusting for potential confounders (adjusted OR 1.52 for highest vs. lowest intake tertile). BPH is not prostatitis, but the two conditions share lower urinary tract symptoms like frequency and urgency. This finding supports the practical recommendation to moderate caffeine if urinary symptoms are a problem (Source 1).
Bottom line: While we don’t yet have definitive causal data for caffeine and prostatitis flares, both clinical experience and related research on urinary symptoms suggest that adjusting caffeine is a sensible, low-risk strategy—especially during symptom flares (Source 1).
How to Cut Back on Caffeine Without Feeling Deprived
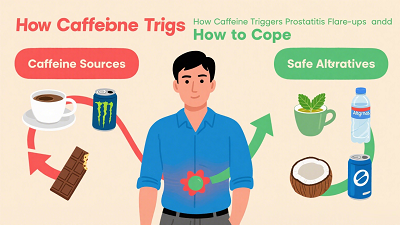
You don’t need to quit caffeine overnight. A smart, gradual approach helps you avoid withdrawal headaches and rebound fatigue while testing how much caffeine your body can handle.
Set a baseline: Track your daily caffeine—coffee, tea, energy drinks, sodas, pre-workout powders, and chocolate. Many people underestimate total intake.
Taper thoughtfully: Reduce by about 25% every 3 to 4 days. For example, move from two large coffees daily to one large and one small, then to two smalls, then to one small.
Time it right: Aim for your last caffeinated beverage before early afternoon to protect sleep quality, a major factor in pain control.
Consider brew methods: Some people find cold brew or darker roasts (which can be lower in perceived acidity) gentler than very bright, acidic coffees. Decaf can still contain small amounts of caffeine, but it’s often well tolerated.
Watch energy drinks: They can pack high caffeine plus additives that may irritate the bladder. If you use them, taper and consider switching to alternatives with known, lower caffeine content.
Test and learn: Once your symptoms settle, reintroduce a small amount of caffeine and see if it remains tolerable.
Smart Beverage Swaps That Are Easier on the Bladder
Decaf coffee or half-caf blends
Herbal teas without known bladder irritants (for many, chamomile or rooibos are gentle; mint or very acidic blends can bother some)
Warm water with a slice of ginger
Low-acid coffee alternatives such as grain-based beverages
Plenty of plain water spaced throughout the day (to avoid concentrated urine that stings) but limit fluid intake a couple of hours before bed or long outings if nocturia or urgency is a problem
Diet Patterns That Support a Calmer Pelvis
The broader eating pattern matters as much as any single beverage. Many men with prostatitis or BPH-like symptoms do better when they emphasize anti-inflammatory, fiber-rich foods and avoid common irritants during flares.
Helpful patterns:
- Pile on vegetables daily, plus a few servings of fruit. Choose a colorful mix for antioxidants.
- Favor plant proteins (beans, lentils, tofu) and fish rich in omega-3s (salmon, sardines).
- Choose whole grains (oats, brown rice, quinoa) to keep bowel movements regular; constipation often worsens pelvic pain.
- Keep weight in a healthy range and stay active most days—both support urinary health and inflammation control.
Common triggers to test-lower during flares:
- Caffeine
- Alcohol
- Very spicy dishes
- High-sodium processed foods
- Sugary foods and sweeteners if you notice symptom spikes
- Large late-night meals and heavy red meat intake
A Symptom-Friendly Sample Day
Breakfast: Oatmeal cooked with almond milk, topped with blueberries and chopped walnuts; herbal tea.
Mid-morning: Low-fat Greek yogurt or a small smoothie with mixed berries and a half-banana.
Lunch: Grilled salmon, a big salad of leafy greens and colorful vegetables, olive oil–lemon dressing; a side of brown rice or quinoa.
Afternoon: Carrots with hummus, or whole-grain crackers with cottage cheese.
Dinner: Grilled chicken breast or a lentil-and-vegetable bowl; steamed broccoli or roasted vegetables.
Evening: Apple slices with a small spoon of peanut butter, or a yogurt parfait with a sprinkle of granola.
Pelvic Floor and Lifestyle Strategies That Reduce Flares
Gentle movement: Brisk walking, easy cycling, or swimming most days can reduce stress and improve urinary function.
Pelvic floor relaxation: Many men with CP/CPPS have a tight, overactive pelvic floor. Diaphragmatic breathing, warm sitz baths, and, when available, pelvic-floor–focused physical therapy can help.
Stress and sleep: Build a wind-down routine, protect 7–9 hours of sleep, and consider relaxation techniques. Good sleep lowers pain amplification.
Bathroom habits: Don’t “push” urine out; allow the bladder to empty with relaxed pelvic muscles. Avoid going “just in case” too frequently, which can train more urgency.
Hydration rhythm: Drink regularly through the day but pull back a couple of hours before bedtime. Don’t over-restrict fluids, which can make urine more concentrated and irritating.
Herbal Support to Prevent Recurring Prostatitis
For men prone to chronic prostatitis flare-ups, combining lifestyle strategies with traditional Chinese medicine can offer additional relief and help prevent recurrence. One option is Diuretic and Anti-inflammatory Pill, an herbal formula known for its diuretic and anti-inflammatory properties. By supporting urinary tract health and reducing inflammation, it can complement dietary adjustments, caffeine moderation, and pelvic floor care.
Many men report fewer flare-ups and improved comfort when using Diuretic and Anti-inflammatory Pill as part of a comprehensive symptom-management plan. Always consult a qualified practitioner before starting any herbal regimen to ensure it fits your individual health profile.
When to See a Clinician
Seek prompt care if you have fever, chills, new severe burning with urination, blood in urine, trouble emptying the bladder, or new severe pelvic pain. These can indicate infection or urinary retention.
For persistent CP/CPPS, ask about a multidisciplinary plan: personalized pelvic floor therapy, pain-modulating strategies, bowel management, and careful review of triggers—including caffeine.
Where the Evidence Leaves Us
We have suggestive evidence that higher caffeine intake is linked to more prostate-related urinary problems in BPH (a condition with overlapping symptoms), supporting caffeine moderation in men with urinary complaints (Source 1).
Direct studies on caffeine and prostatitis flares are limited, so the best approach is a personalized experiment: taper caffeine, track symptoms, then reintroduce small amounts to identify your safe zone.
Pair caffeine moderation with an overall symptom-friendly diet, good sleep, stress reduction, and pelvic floor relaxation for the best results.
Practical Next Steps
- Track your caffeine and symptoms for one week.
- Taper caffeine by 25% every 3–4 days while substituting gentler beverages.
- Adopt a fiber- and omega-3–rich meal pattern and reduce common irritants during flares.
- Add daily gentle exercise and a sleep routine.
- If symptoms persist or red flags appear, see your clinician for evaluation and a tailored treatment plan.
References
Frontiers in Nutrition (2024). Exploring the association between caffeine intake and benign prostatic hyperplasia: results from the NHANES 2005–2008



