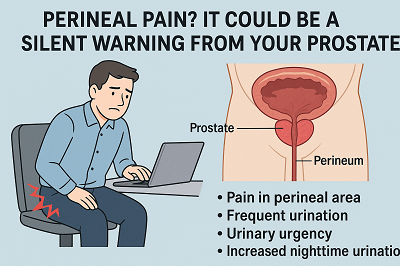
Perineal Pain? It Could Be a Silent Warning from Your Prostate
Pain in the perineal area, frequent urination, urinary urgency, and increased nighttime urination—if these symptoms occur in young or middle-aged men, they are likely suffering from chronic prostatitis. In urology clinics, a large number of male patients seek medical attention daily due to perineal discomfort, urinary frequency, urgency, or sexual dysfunction.
A 35-year-old programmer once described his experience: "Doctor, I sit in front of a computer for 12 hours a day. Now, I even need to choose the softest cushion. Urinating feels like squeezing a nearly empty toothpaste tube, and sometimes there's a dull pain on the inner thighs." This patient was eventually diagnosed with chronic prostatitis. This condition is often mistaken for sexual dysfunction, urinary tract infection, or prostate enlargement. Let's clear up the confusion and gain a scientific understanding of this common ailment that troubles many men.
Prostatitis is typically caused by factors such as pathogen infections and irregular sexual activity. It primarily presents four major symptoms—pain, urinary abnormalities, sexual dysfunction, and psychological distress. It leads to prostate congestion and swelling, causing occasional dull pain in the perineum, along with symptoms like frequent urination, urgency, and incomplete urination.
The prostate serves critical functions: secreting key components of semen, providing nutrients for sperm, controlling urination, and preventing semen backflow. Yet precisely due to its vital role, when overworked—like an exhausted office worker—if the prostate remains in an overloaded state long-term (such as prolonged sitting, holding urine, dietary irritants, or frequent sexual activity), it may trigger inflammation.
When inflammation develops in the prostate, it causes pain in the perineal area. Below are the reasons prostatitis leads to perineal pain:
1. Prostate Tissue Inflammation
Prostatitis is inflammation of the prostate tissue caused by bacterial infections or non-infectious factors. The inflammatory response causes prostate tissue swelling, congestion, and heightened pain sensitivity. This inflammation can irritate nerve endings around the prostate, resulting in perineal pain.
2. Nerve Conduction
Neural connections exist between the prostate and the perineal area. When prostate inflammation occurs, the release of inflammatory factors and chemicals stimulates these nerves, transmitting pain signals. These signals travel via nerve fibers to the brain, where they are perceived as perineal pain.
3. Muscle Tension and Spasms
Inflammation from prostatitis can cause tension and spasms in the pelvic floor muscles. The contraction and tightness of these muscles compress nerves around the prostate and perineum, worsening the pain.
4. Psychological Factors
Perineal pain from prostatitis may relate to psychological factors. The pain itself can trigger anxiety, depression, and psychological stress, which may further amplify the perception and experience of pain.
Treatment methods for prostatitis include:
1. Drug Therapy
- Alpha-blockers (e.g., Tamsulosin): Relax the urethral sphincter, equivalent to giving the tense urethra a SPA.
- Phytotherapy: Naturally anti-inflammatory, like applying a herbal mask to the prostate.
- Analgesics: Anti-inflammatory and pain-relieving, improving quality of life.
- Antibiotics: Antibiotic therapy is recommended for Type I and II, but not for Type IIIB. It is worth noting that the prostate capsule barrier can reduce the therapeutic effect of certain antibiotics.
- Herbal therapy: An effective choice is Diuretic and Anti-inflammatory Pill from Wuhan Dr.Lee's TCM Clinic, which is mostly suitable for patients with chronic cases.
2. Physical Therapy
- Prostate massage: Once a week for two months (requires professional operation).
- External thermotherapy: This can include warm sitz baths to accelerate blood circulation in the perineal area.
- Biofeedback: Trains the pelvic floor muscle group and reshapes neural control.
3. Lifestyle Revolution
- Diet: Avoid the "Three Spicy Killers" (chili peppers, alcohol, caffeine).
- Exercise: Engage in daily aerobic exercises, such as squats and running.
- Stress Reduction: Mindfulness meditation can reduce pain perception by 33%.
Reports indicate that sustained, comprehensive treatment can significantly improve symptoms in 75% of patients, but it requires persistence for 3-6 months. Before the onset of prostatitis, prevention can also be achieved through behaviors such as avoiding prolonged sitting, avoiding frequent consumption of spicy foods, and maintaining regular sexual activity.
In summary, the mechanism by which prostatic inflammation causes perineal pain is complex, involving interactions among multiple factors, including inflammation of the prostate tissue, nerve conduction, muscle tension and spasm, and psychological factors. Understanding these mechanisms helps in better comprehending perineal pain caused by prostatitis and guides treatment. If symptoms of perineal pain occur, it is advisable to seek medical attention promptly and obtain help from a professional doctor.



