Intervention Strategies for Premature Ejaculation in Patients with Benign Prostatic Hyperplasia and Chronic Inflammation
Benign prostatic hyperplasia (BPH) commonly affects aging men and often coexists with chronic prostatitis or chronic pelvic inflammation. While urinary symptoms such as urgency and nocturia dominate clinical presentations, many patients also report sexual dysfunction, particularly premature ejaculation (PE).
This article explores the pathophysiological connections between BPH, chronic inflammation, and PE, and presents a multifaceted intervention strategy, including natural treatment options, behavioral therapies, and psychological support.
Understanding the Link: Why BPH with Inflammation Triggers PE
PE in men with BPH and chronic prostatitis is typically a result of overlapping physical and psychological mechanisms:
Neurogenic Inflammation and Pelvic Sensitization
Chronic inflammation in the prostate can trigger long-term activation of pelvic sensory nerves, lowering the threshold for ejaculation. Studies have shown that chronic pelvic pain syndrome (CP/CPPS), a subtype of prostatitis, is closely associated with heightened pelvic floor tension and altered nerve signaling, which in turn leads to ejaculatory dysfunction.
Pelvic Floor Dysfunction
Persistent discomfort in the perineal or prostate region can lead to pelvic floor muscle hypertonicity. This tension may contribute to involuntary muscular contractions and reduced ejaculatory latency.
Psychological and Emotional Stress
Chronic genitourinary symptoms are often linked with anxiety, depression, and sexual performance pressure, all of which are known contributors to PE. Patients may also experience a fear of pain or worsening urinary symptoms after ejaculation, leading to anticipatory anxiety.
A 2013 review by Shoskes et al. found that sexual dysfunction was present in more than 50% of patients with CP/CPPS, highlighting the strong correlation between chronic prostate inflammation and premature ejaculation, among other issues [1].
Key Symptoms to Identify
Patients with BPH and chronic inflammation-related PE often report:
- Rapid ejaculation with minimal stimulation
- Perineal or urethral discomfort after ejaculation
- Anxiety or avoidance of sexual activity
- Worsening of PE during prostatitis flare-ups
These symptoms significantly impact sexual confidence and quality of life, making effective management essential.
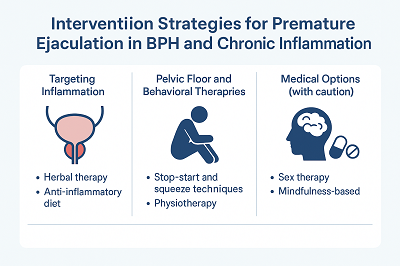
Comprehensive Intervention Strategies
1. Targeting Inflammation as the Root Cause
Herbal Therapy: Diuretic and Anti-inflammatory Pill
This traditional Chinese herbal formula is designed to clear heat, eliminate dampness, improve blood circulation, and reduce swelling in the prostate. Many patients have reported improvements in both urinary symptoms and sexual function after 1–3 treatment courses.
The Diuretic and Anti-inflammatory Pill works by:
- Alleviating chronic inflammation and pelvic congestion
- Supporting healthy prostate secretion and circulation
- Improving sperm quality and overall sexual performance
To learn more, visit: www.diureticspill.com
Anti-inflammatory Diet
Include foods rich in zinc (e.g., pumpkin seeds), omega-3 fatty acids (e.g., salmon), and anti-inflammatory spices like turmeric. Avoid caffeine, alcohol, and spicy foods that may irritate the prostate.
2. Pelvic Floor and Behavioral Therapies
Kegel Exercises and Pelvic Muscle Relaxation
Restoring control over the pelvic muscles can help delay ejaculation and reduce post-ejaculatory discomfort.
Stop-Start and Squeeze Techniques
These methods retrain the ejaculatory reflex and can be effective for regaining control in men with secondary PE.
Physiotherapy
Targeted pelvic physiotherapy has been shown to reduce pain and improve ejaculatory control in men with CP/CPPS.
3. Psychological Interventions
Sex Therapy and Cognitive Behavioral Therapy (CBT)
Psychological counseling can help address underlying stress, negative sexual expectations, and anxiety. Incorporating a partner into therapy can further enhance outcomes.
Mindfulness-Based Approaches
These techniques help patients stay present during intimacy and avoid performance anxiety—a known trigger of PE.
A meta-analysis in 2025 found that approximately 35% of men with chronic prostatitis also suffer from PE, reinforcing the importance of psychological and neuroinflammatory pathways in its development [2].
4. Conventional Medical Options (with Caution)
Alpha-blockers (e.g., Tamsulosin)
May help relieve urinary obstruction and pelvic tension, indirectly improving sexual function.
SSRIs (e.g., Paroxetine)
Sometimes used off-label for delaying ejaculation. However, side effects such as fatigue and libido reduction are common, making them less ideal for long-term use.
Lifestyle Modifications That Support Recovery
- Regular exercise boosts circulation and testosterone levels
- Stress management through meditation or yoga can lower inflammation
- Adequate sleep and hydration support immune and hormonal balance
Conclusion
Premature ejaculation in men with BPH and chronic prostatitis is a treatable condition. Addressing both the inflammatory and psychological components is key to successful intervention. A combination of natural herbal therapy, pelvic rehabilitation, and behavioral techniques offers the most comprehensive and sustainable relief.
The Diuretic and Anti-inflammatory Pill, with its anti-inflammatory and prostate-regulating properties, provides a valuable non-invasive treatment alternative for men seeking to restore sexual health without side effects.
References
1. Shoskes DA, Nickel JC. Sexual dysfunction in chronic prostatitis/chronic pelvic pain syndrome. World J Urol. 2013;31(4):741–746. DOI: 10.1007/s00345-013-1076-5
2. Alshahrani S, Fathi BA, Abouelgreed TA, El‑Metwally A. Prevalence of Sexual Dysfunction with Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS): An Updated Systematic Review and Meta‑Analysis. Medicina. 2025;61(6):1110. DOI: 10.3390/medicina61061110



